General information only; not personal medical advice. Follow your clinic’s post‑sedation and recovery instructions.
Featured answer
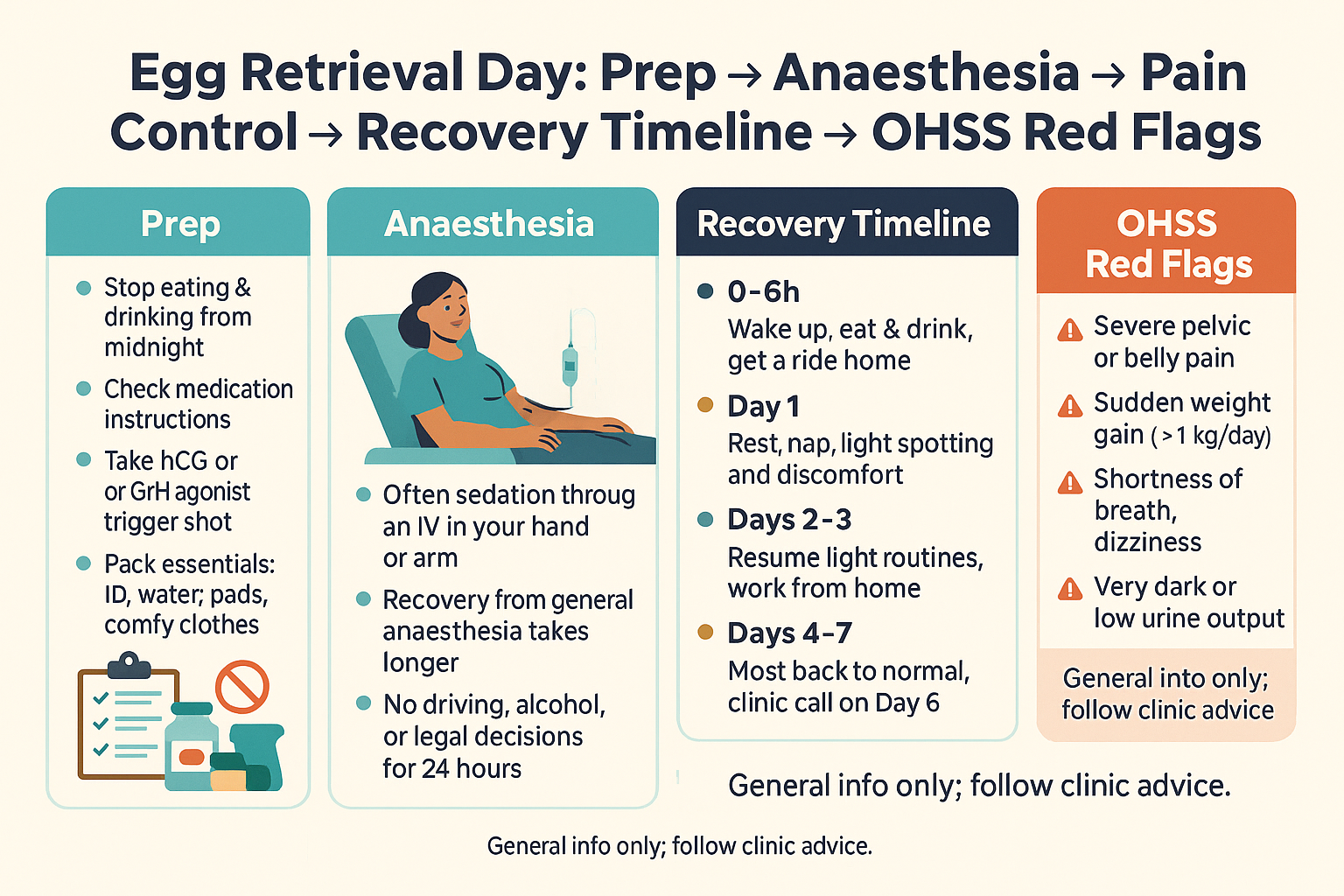
Most people feel crampy and bloated for 1–3 days after egg retrieval, improving by day 3–5. Rest, fluids, and simple pain relief help. Avoid driving, alcohol, and heavy activity for 24 hours after sedation. Call your clinic urgently for rapid weight gain, severe or one‑sided pain, shortness of breath, faintness, or very low urine.
Introduction
Nerves before retrieval are normal. You may be wondering about anaesthesia, how painful recovery feels, and how much time off work you need. This guide gives a calm, practical map for egg retrieval recovery with clear safety cues.
We cover sedation vs general anaesthesia, trigger timing, pain control, bowel care, and day‑by‑day expectations. Egg retrieval recovery varies by clinic and country, but common steps are similar.
Egg Retrieval Recovery at a Glance
What the procedure involves in plain English
Eggs are collected with a thin needle passed through the vaginal wall under ultrasound guidance. Follicle fluid is aspirated; the embryology team finds oocytes in the lab. This is often called oocyte pick‑up (OPU).
Typical symptoms and how long they last
Cramping, bloating, and spotting are common for 1–3 days. Soreness tends to increase with the number of follicles aspirated, then settles by day 3–5. Shoulder‑tip pain is uncommon and should improve quickly.
Common mistake: doing too much in the first 24–48 hours
Post‑sedation, most clinics ask you to rest at home, avoid driving, alcohol, heavy lifting, and important decisions for 24 hours. Overdoing it can prolong cramping and bloating.
Evidence: ASRM OHSS guidance (2016) notes symptom peaks within the first week; ASA procedural sedation guidance (2018) advises no driving and supervision for 24 hours.
Prep Checklist (The Day Before and Morning Of)
Fasting/NPO rules and medication checks
Most clinics use IV conscious sedation. Typical rules: no solid food for 6 hours and no clear fluids for 2 hours before arrival. Take only medicines approved by your team. Ask about aspirin/NSAIDs, metformin, and inhalers. Bring your ID and consent forms.
Trigger timing (hCG vs GnRH agonist) and why it matters
The trigger is timed to start final oocyte maturation. hCG triggers can raise OHSS risk; GnRH‑agonist triggers lower risk in antagonist cycles. The shot is usually 34–36 hours before OPU. Set alarms and confirm the exact time with staff.
Pack list and home set‑up (Retrieval packing list)
Phone charger, pads (not tampons), comfy clothes, water bottle, simple snacks, heat pack, approved pain relief, electrolyte drink, and a ride home. At home, set up bedding near the bathroom and keep a notepad for urine, weight, and symptoms.
Evidence: ESHRE ovarian stimulation guidance (2019) supports agonist trigger for high‑risk OHSS.
Anaesthesia 101 (Sedation vs General)
What IV conscious sedation feels like
You get an IV, oxygen by nasal prongs, and continuous monitoring. Most people feel drowsy and remember little. You can breathe on your own and recover faster than with general anaesthesia.
Safety basics and post‑sedation rules
You need a responsible adult for the day. No driving, alcohol, important legal documents, or heavy activity for 24 hours. Expect a call or review before discharge.
When clinics use general anaesthesia
Some centers use general anaesthesia based on policy, past anaesthetic history, or complex anatomy. Recovery may take longer. The procedure is the same.
Evidence: ASA Moderate Procedural Sedation guideline (2018); clinic anaesthesia FAQs (Illume Fertility 2023) outline typical post‑sedation rules.
Pain Control, Bloating, and Bowel Care
Over‑the‑counter options and clinic‑approved meds
Discuss options with your clinic. Many approve paracetamol/acetaminophen. Some allow NSAIDs after OPU; others avoid them if fresh transfer is planned. Use opioids only if prescribed. Avoid aspirin unless directed.
Heat, hydration, electrolytes, gentle movement
Use a warm (not hot) heat pack for cramps. Aim for regular fluids and small, salty meals if you feel light‑headed. Electrolyte drinks can help if you are queasy. Short walks help gas pain and prevent stiffness.
Constipation prevention after sedation and opioids
Start fibre, fluids, and a gentle stool softener the day of retrieval if you are prone to constipation or were given opioids. Avoid straining.
Evidence: Cochrane reviews of analgesia for oocyte retrieval and post‑procedure recovery (2013–2017) support multi‑modal pain control.
Recovery Timeline (Hour‑by‑Hour / Day‑by‑Day)
0–6 hours: waking up, first food/fluids, ride home
You may feel groggy and crampy. Start with sips of water, then light food. Pee before you leave. No driving. Rest with supervision.
Day 1: rest plan, pain scale expectations
Expect period‑like cramps (2–5/10) and bloating. Spotting is common. Use heat and clinic‑approved pain relief. Keep a symptom log.
Day 2–3: light activity, work‑from‑home guidance
Many feel better by day 2–3. Light tasks and short walks are fine. Many can work from home; desk jobs often resume on day 2 or 3.
Day 4–7: gradual return to normal; gym/sex/travel cautions
Slowly return to usual activity. Avoid high‑impact exercise, heavy lifting, and intercourse until your clinic clears you. Ovaries are still enlarged.
Comment: How many oocytes did you have retrieved, and on which day did you feel “back to normal”? Share below to help others.
| Time window | What to expect | What to do |
|---|---|---|
| 0–6 h | Drowsy, cramps, spotting | Sip fluids, eat light, no driving |
| Day 1 | Bloating, period‑like cramps | Heat pack, approved pain relief, rest |
| Day 2–3 | Improving soreness | Short walks, light work from home |
| Day 4–7 | Near baseline | Gradual return; avoid heavy gym/sex until cleared |
OHSS After Retrieval—Know the Windows
Early vs late OHSS; why late can follow trigger or pregnancy
Early OHSS shows within 3–5 days after trigger and is linked to the trigger shot. Late OHSS can appear a week or more later if pregnancy hormones rise. Risk is higher with many follicles, high estradiol, and hCG trigger.
Self‑monitoring: weight, waistline, urine output
Weigh daily at the same time. Track waistline at the navel. Note urine output and color. Call if you gain >1 kg (2 lb) in 24 hours or 2–3 kg (4–6 lb) in 72 hours, have severe bloating, or very low urine.
When to call vs when to seek urgent care
Call your clinic promptly for worsening pain, distension, or reduced urine. Seek urgent care for shortness of breath, chest pain, faintness, severe one‑sided pain, or rapid weight gain with minimal urine.
Evidence: ASRM OHSS prevention/management (2016; reaffirmed updates) describes early/late windows and red‑flag escalation.
When to Resume Normal Life
Driving, work, lifting, exercise, intercourse, tampons vs pads
No driving for 24 hours post‑sedation. Many return to desk work by day 2–3. Avoid heavy lifting and high‑impact workouts for a week or as advised. Avoid intercourse until ovaries settle; use pads, not tampons, while spotting.
Travel and altitude notes post‑sedation and if OHSS risk is high
Avoid solo travel in the first 24 hours. If you are high risk for OHSS, delay flights until symptoms are clearly improving and you have clinic clearance.
Follow‑up calls and when you’ll hear fertilisation updates
Most labs call the same day or next morning with fertilisation results, then give a day‑by‑day update plan. Ask when luteal support starts.
Evidence: Clinic recovery pages and ESHRE (2019) highlight activity limits until ovaries shrink.
Proof & Practicals
Mini case snapshot
High‑oocyte count retrieval with swollen feeling and tight waistband through day 3. Hydration, electrolytes, short walks, and heat pack used. By day 5, bloating eased and pain was 1–2/10. No red flags. Returned to office work on day 3.
48‑Hour Post‑Retrieval Plan
- Rest at home with supervision for 24 hours.
- Fluids + electrolytes; small, salty snacks if light‑headed.
- Clinic‑approved pain relief; warm heat pack.
- Gentle walks every few hours; avoid heavy lifting.
- Track weight, waistline, urine.
- Use pads for spotting; no tampons or intercourse.
- Save your clinic’s on‑call number.
If you’re at higher OHSS risk
Ask about agonist trigger, cabergoline, or freeze‑all. Weigh daily. Call early for rapid changes. See our guide: OHSS symptoms and what to do.
FAQ
How painful is egg retrieval recovery and for how long?
What anaesthesia is used for egg retrieval?
What can I take for pain after retrieval?
What are normal symptoms vs warning signs after egg retrieval?
When can I go back to work or exercise?
Can I drive or travel after sedation?
How do I know if I’m developing OHSS?
Conclusion
Egg retrieval recovery is usually a few crampy, bloated days that ease by day 3–5. Rest, fluids, and simple pain control work well for most. Know the OHSS windows and call promptly for red flags. Follow your clinic’s post‑sedation and recovery instructions.
Sources
- ASRM: Prevention and treatment of moderate and severe ovarian hyperstimulation syndrome (2016) — guidelines by ASRM Practice Committee.
- ESHRE: Guideline on ovarian stimulation for IVF/ICSI (2019) — guideline from the European Society of Human Reproduction and Embryology.
- ASA: Practice Guidelines for Moderate Procedural Sedation (2018) — anaesthesia society guidance on post‑sedation care and safety.
- Illume Fertility: Egg Retrieval Anesthesia FAQs (2025) — clinic FAQ on what sedation feels like and recovery rules.
- Cochrane Library: Analgesia for oocyte retrieval (2013–2017) — review articles on pain control strategies.
Reminder: Follow your clinic’s instructions. Seek urgent care for severe symptoms.