Featured answer
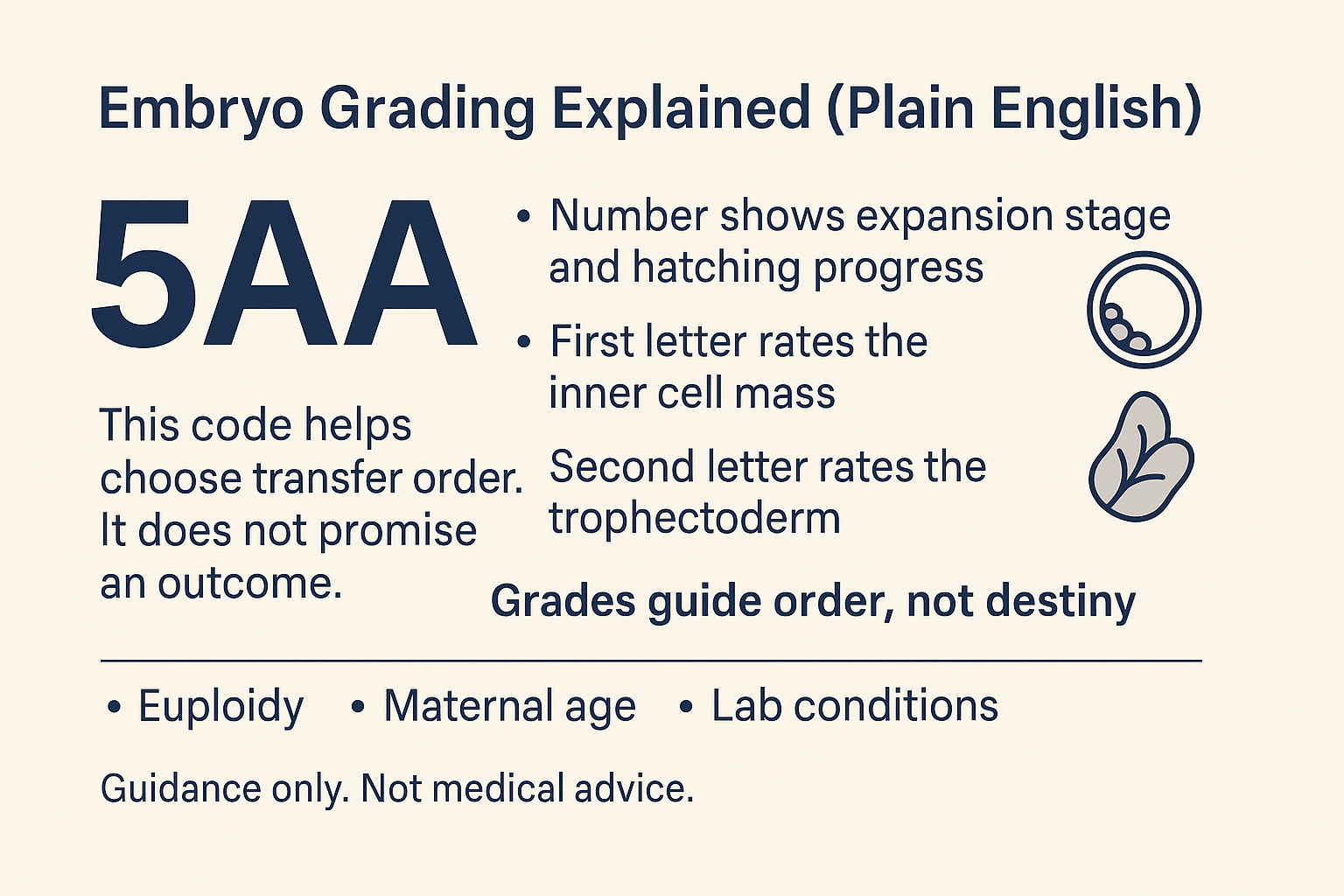
Here is embryo grading explained in plain English. In a blastocyst grade like 5AA, the number shows expansion stage and hatching progress. The first letter rates the inner cell mass. The second letter rates the trophectoderm. This code helps choose transfer order. It does not promise an outcome. Euploidy, maternal age, and lab conditions also matter.
Introduction
Seeing 5AA or 3BB can feel like alphabet soup. You want a simple way to read the report without overthinking it. This guide gives embryo grading explained with a clear decoder and a fair look at what predicts success.
We cover Day 3 vs Day 5 grading, the Gardner chart, ICM vs TE, and why grades guide order, not destiny. Evidence is drawn from Human Reproduction cohorts, NEJM reviews, and large clinic series.
Embryo Grading Explained in 60 Seconds
The code — numbers vs letters
Numbers show expansion stage. Letters grade the inner cell mass and the trophectoderm. Most clinics use the Gardner and Schoolcraft system for blastocysts.
What each part means
- Expansion 1 to 6: early to fully expanded or hatched.
- ICM A to C: size and compactness of the inner cell mass.
- TE A to C: layer of outer cells that form the placenta.
Common mistake: treating grades as guarantees
Grades help rank embryos. They do not prove an embryo is chromosomally normal or that it will implant.
Evidence: Large cohorts link higher morphology with higher implantation, but live birth also depends on euploidy and age (Human Reproduction 2019; NEJM 2016).
Decoding Examples (With Plain‑English Translations)
- 5AA: fully expanded with strong ICM and TE. Often high priority if age and context fit.
- 4AB: expanded with strong ICM and good TE. A common top choice.
- 3BB: early blastocyst with good ICM and TE. Many succeed, especially if euploid.
- 2BC: very early blast with smaller ICM and fair TE. May need more time or may be frozen if suitable.
- D6 3BA: early blast on Day 6 with strong ICM and good TE. Often used if euploid.
- D7 4BB: expanded on Day 7 with good ICM and TE. Some clinics use with care; policies vary.
Why a 4AB may be chosen over a 3AA sometimes
Expansion stage can matter for timing. A slightly lower letter grade with more expansion may be picked for transfer in some labs.
Poor‑grade successes
Clinic cohorts show that lower grades still yield pregnancies. Grades guide order. They do not rule out healthy babies.
Which grade on your report ended up surprising you, better or worse than expected?
Day 3 vs Day 5/6/7 (What’s the Real Difference?)
Cleavage‑stage measures
Day 3 looks at cell number and fragmentation. It is a quicker snapshot. Grading terms differ from blastocysts.
Blastocyst advantages and timing realities
Day 5 to 7 grading allows ICM and TE assessment. Not every embryo reaches blastocyst by Day 5. Some need Day 6 or 7.
Fresh vs frozen context; vitrification survival
Freezing is common today. Vitrification survival is high in modern labs. Local numbers vary.
Evidence: Modern vitrification yields high survival and similar outcomes versus fresh in many settings (NEJM 2016 review; Human Reproduction 2018 cohort).
What Actually Predicts Success
Maternal age and euploidy odds
Age and chromosome status drive outcomes more than letters alone. Use grades with the age context of the cohort.
PGT‑A interplay
If embryos are tested, clinics still use morphology to rank euploid embryos for transfer order.
Lab variation and culture
Culture conditions and policies differ across clinics and countries. Staff experience matters.
Evidence: Morphology predicts implantation within age groups, but euploidy status is the stronger driver of live birth (Human Reproduction 2019; NEJM 2016).
ICM vs TE — Which Matters More?
Evidence snapshot
Several cohorts suggest both matter. Some find ICM has a stronger link to live birth, while others see TE driving implantation. Results vary.
Practical ranking when letters disagree
If 4AA, 4AB, and 4BA are available, many labs pick 4AA, then weigh ICM and TE with expansion and timing.
D6 vs D5 nuance
Some studies find slightly lower outcomes with Day 6 vs Day 5 in untested cohorts. The difference narrows among euploid embryos. Day 7 use varies.
Evidence: Human Reproduction 2018 and large clinic series report D6 vs D5 differences that shrink after PGT‑A.
From Report to Plan: How Clinics Use Grades
Transfer order vs discard myths
Grades help order decisions. They do not equal keep vs discard. Clinics judge the full picture and may re‑assess after warming.
When to consider freezing, biopsy, or waiting to D6/D7
This depends on age, cohort size, and clinic policy. Ask about local data.
Questions to ask your clinic
What is our embryo’s code and plain English meaning. How do you rank embryos like ours. How do age and testing change the plan.
Evidence: Clinic data and Human Reproduction series support a ranking system that includes expansion, ICM, and TE, with age and testing layered in.
Proof & Practicals
Mini case snapshot
A 3BB Day 6 embryo led to a healthy birth after a lower‑grade sibling was transferred first. Order helped planning. Destiny was not fixed by letters.
Blastocyst Grading at a Glance
| Aspect | Code | Plain English |
|---|---|---|
| Expansion | 1–6 | Early to fully expanded or hatched |
| ICM | A / B / C | Cell mass quality in the embryo |
| TE | A / B / C | Outer layer that forms the placenta |
Checklist: How to read your embryo report
- Find the expansion number.
- Read the ICM letter.
- Read the TE letter.
- Note the day: D5, D6, or D7.
- Ask how your clinic ranks letters when they disagree.
- Add age and testing context.
- Plan next steps with your team.
Grades vs outcomes
Grades guide order. Outcomes follow biology and care. Learn more in our explainer: Grades vs outcomes and try the Embryo grade viewer.
FAQ
What does 5AA or 3BB mean in embryo grading?
Is Day 5 always better than Day 3?
Which matters more, ICM or TE?
Do higher grades guarantee a higher live birth rate?
Can a poor‑grade embryo still implant?
How does PGT‑A relate to grading?
Do frozen embryos change grade or chances?
Conclusion
This is embryo grading explained in plain English. Grades help order embryos for transfer and storage. They do not make promises. Age, euploidy, and lab conditions drive outcomes. Ask your team to translate your report and plan next steps.
Sources
- NEJM: Transfer of Fresh vs Frozen Embryos in Ovulatory Women (2018) — landmark RCT informing modern outcomes on fresh vs frozen transfer strategies.
- Fresh Day-5 slow-growing vs deferred vitrified Day-6 blastocysts (2019) — cohort analyses within 2019 issues.
- Effect of denudation/injection timing on ICSI outcomes (2020) — large single-centre cohort on timing and results.
- Embryo morphokinetics and maternal age (2019) — time-lapse cohort linking timing parameters with outcomes.
- ASRM: Comprehensive guidance for embryology/andrology/endocrinology labs (2022).
- ARCS: Good practice in clinical embryology laboratories (2024) — updated UK lab practice guidance.
- Cochrane: Fresh vs frozen embryo transfer evidence summary — high-level review on FET vs fresh outcomes.
Reminder: Discuss your report with your fertility team before making decisions about transfer or storage.