Featured answer
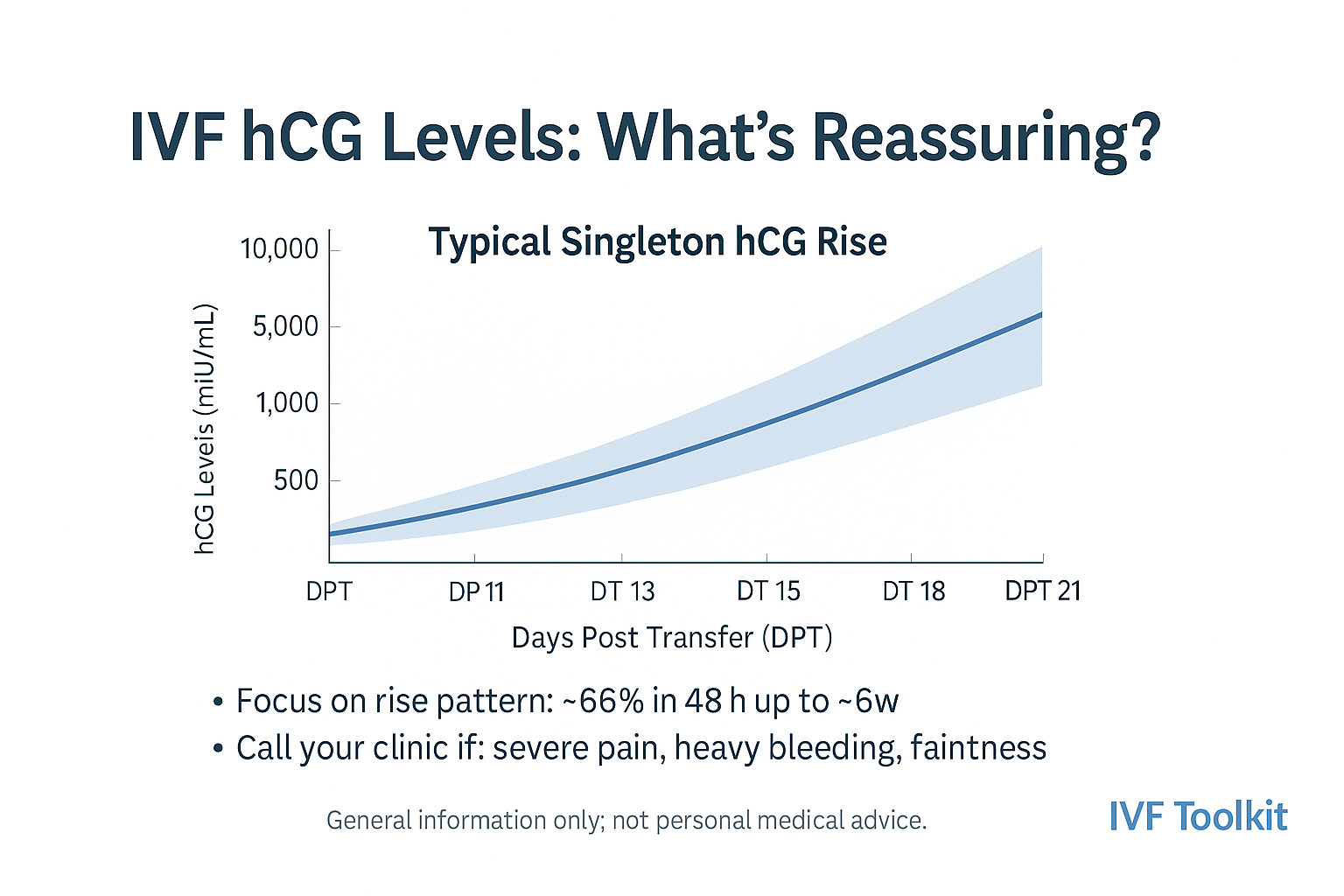
Reassuring IVF hCG levels show a steady rise over 48 to 72 hours. A common clinical rule is at least a 35 percent rise in 48 hours up to 6 weeks, with many singletons rising 60 to 100 percent. Typical early ranges vary by day‑of‑transfer and lab. Repeat the beta in 48 hours. Call your clinic sooner if you have red‑flag symptoms.
Introduction
You got a result and now you are searching charts. The right way to read IVF hCG levels is to watch the rise. The exact number matters less than the pattern. In this guide you will see simple ranges by DPT, the rise most services expect, how to time ultrasound, and when to call.
IVF hCG Levels 101 (What β‑hCG Measures)
Why this matters
β‑hCG is made by trophoblast cells after implantation and supports the corpus luteum. Levels start low and then climb fast in early weeks. Clinicians use the change in 48 to 72 hours to judge early trends (RANZCOG 2023; RACGP 2021).
How to interpret units and labs
Results are in mIU/mL. Different labs use different assays. Numbers from two labs may not match. Try to use the same lab for repeats. Always note the DPT and transfer day (D3 vs D5).
Common mistake (chasing absolute numbers)
A modest first beta can still be fine if the rise is appropriate.
Evidence: Viable early pregnancies can rise as little as 35% in 48 hours up to 6 weeks (Barnhart 2004; NICE 2019).
What Numbers Are Reassuring by DPT (Day‑3 vs Day‑5)
Typical ranges and variability
| DPT | Day‑5 transfer singleton | Day‑3 transfer singleton | Notes |
|---|---|---|---|
| 9 | 50–120 mIU/mL | 30–90 mIU/mL | wide scatter |
| 10 | 80–180 | 50–140 | pattern matters more |
| 12 | 150–400 | 100–300 | many double here |
| 14 | 300–800 | 200–600 | ultrasound planning next |
Twins tend to be higher, but there is large overlap. Only ultrasound confirms number.
How to do it: plan repeat testing
- Record your DPT and transfer type.
- Repeat the beta in 48 hours with the same lab.
- Look for at least a 35% rise. Many will rise 60–100%.
- Keep context. Symptoms and timing matter.
Mistake: comparing to non‑IVF charts
Many public charts use LMP timing. IVF uses DPT. Do not cross‑compare.
Evidence: RACGP and ACOG note rate‑of‑rise helps triage but ultrasound confirms location once hCG is high enough.
Doubling Time vs 48‑Hour Rise (What Clinicians Look For)
Why this works
In early viable pregnancies, hCG rises along a curve and slows with time. By 6–7 weeks the curve starts to flatten. Rate‑of‑rise is more useful than a single value.
How to calculate doubling time
Doubling time (hours) = time between tests × 0.693 ÷ ln(hCG2 ÷ hCG1).
Example: 48 hours from 120 to 240 → about 48 hours.
Mistake: expecting exact 48‑hour doubling every time
Many viable pregnancies do not double in 48 hours. A 35–53% rise in 48 hours can be normal up to 6 weeks. The curve slows after that.
Evidence: Barnhart 2004 lower‑bound rise replicated in later cohorts.
Plateaus, Slow Rises, and When to Call Your Clinic
Patterns that need follow‑up
- Rise < 35% in 48 hours up to 6 weeks
- Falling levels over two tests
- Persistent pain or bleeding regardless of number
- hCG above local scan threshold without a sac on scan
Red‑flag symptoms (urgent)
Sharp one‑sided pain, shoulder tip pain, faintness, heavy bleeding, or rapid change in symptoms. Seek urgent care.
Mistake: waiting a week to re‑test
In early weeks, 48 hours gives the most useful trend.
Evidence: RANZCOG 2023 and NICE 2019 advise fast follow up for possible ectopic or pregnancy of unknown location.
Special Situations (Twins, Biochemical, Ectopic, Trigger, Hook Effect)
Twins and higher values
Twins often start higher and rise faster. Overlap is common. Never assume twins based on hCG alone.
Biochemical pregnancy
A small rise that then falls. Your team will guide next steps.
Ectopic clues and next steps
Slower rise, pain, and no sac when levels are above the local scan threshold. Needs imaging and clinical review.
Trigger shot and hook effect (rare)
A trigger can affect very early tests. The hook effect is rare and fixed by dilution at the lab.
From Beta to Ultrasound: Timing the First Scan
Discriminatory zone and expectations
Many services expect a sac to be seen on high quality transvaginal ultrasound when hCG is around 1500 to 3500 mIU/mL. Thresholds vary by machine and operator.
How to schedule and what to look for
Most book the first scan at about 6–7 weeks. Expect a sac, a yolk sac, then a fetal pole with cardiac activity. Timing varies.
Mistake: over‑scanning too early
Early scans may only create worry. Your team will time the scan.
Comment: What was your first beta and DPT. Share below so others can compare.
Proof & Practicals
Mini case
12 DPT after a D5 transfer. First beta 110 mIU/mL on 17 September 2025. Repeat at 14 DPT was 220. Rise 100% in 48 hours. Scan at 6+4 showed a single live intrauterine pregnancy.
Example rise table
| DPT | Singleton example | Twins example |
|---|---|---|
| 9 | 60 | 120 |
| 11 | 150 | 300 |
| 13 | 320 | 700 |
| 15 | 650 | 1400 |
Checklist: what to do after your first beta
- Write down DPT and transfer type.
- Book a repeat in 48 hours with the same lab.
- Use a doubling time calculator to check rise.
- Watch for red‑flag symptoms.
- Plan the first scan with your clinic.
- Keep notes in the hCG Tracker.
- Ask if results came from different labs.
Myth vs Fact
Myth: High hCG always means twins.
Fact: Twins often run higher, but overlap is large. Only ultrasound confirms number.
FAQ
What IVF hCG levels are normal at 9 to 14 DPT
How fast should beta hCG rise after IVF
Does a low first beta still lead to a healthy pregnancy
When does hCG plateau and is that normal
What is the difference between absolute value and doubling time
Can the hCG trigger or hook effect affect results
When should I repeat beta or book ultrasound
Conclusion
IVF hCG levels make more sense when you watch the rise, not just the number. Aim for at least a 35 percent rise in 48 hours in early weeks. Plan your scan at the right time. If something feels off, call your clinic.
CTAs
- Log your numbers in the hCG Tracker and share your DPT and first beta in the comments: https://ivftoolkit.com/hcg-tracker
- Bookmark this guide and check back after your next beta.
Reminder: If you have pain, heavy bleeding, faintness, or rapid hCG changes, contact your fertility unit or emergency care.
Sources
- RANZCOG: Early pregnancy care (2023) — clinical practice guidance from the Royal Australian and New Zealand College of Obstetricians and Gynaecologists.
- RACGP: Early pregnancy bleeding (2021) — guidance for general practice management in Australia.
- NICE: Ectopic pregnancy and miscarriage (2019) — UK evidence-based guidelines from the National Institute for Health and Care Excellence.
- ACOG: Early pregnancy loss (2018 update) — practice bulletin from the American College of Obstetricians and Gynecologists.
- Barnhart K. Clinical factors affecting initial hCG rise (2004). Fertility and Sterility. — peer-reviewed research article (no public link available).