General information only; not personal medical advice. Follow your clinic’s luteal support protocol. Do not change dose or route without clinician guidance.
Featured answer
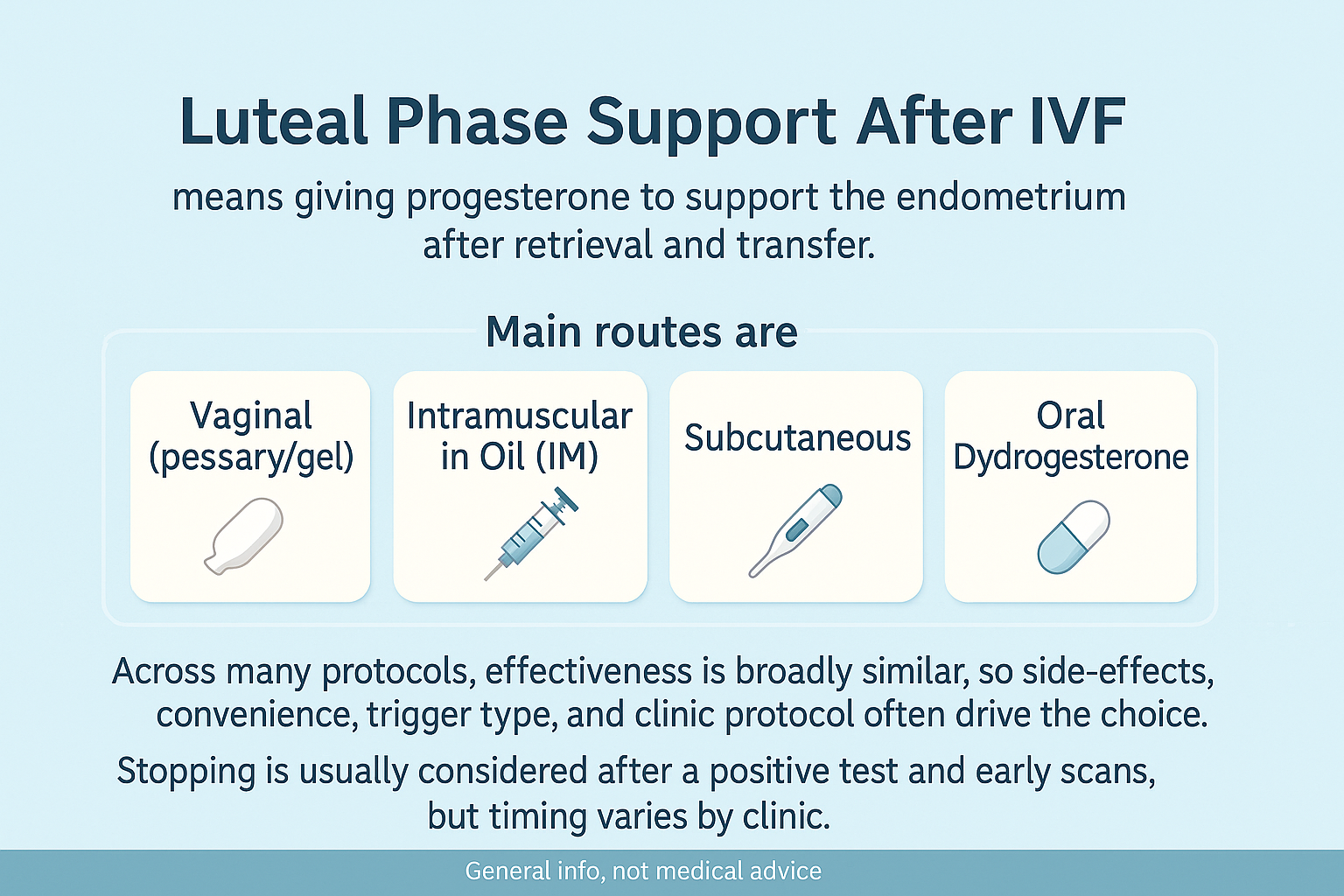
Luteal phase support after IVF means giving progesterone to support the endometrium after retrieval and transfer. The main routes are vaginal (pessary/gel), intramuscular in oil (IM), subcutaneous aqueous progesterone, and oral dydrogesterone. Across many protocols, effectiveness is broadly similar, so side‑effects, convenience, trigger type, and clinic protocol often drive the choice. Stopping is usually considered after a positive test and early scans, but timing varies by clinic.
Introduction
“Which progesterone should I use?” is a common question. This guide lays out luteal phase support IVF in plain English. We compare routes, side‑effects, and timing, and highlight what recent studies and guidelines say.
You will see why many clinics reach similar outcomes with different routes, how trigger type changes support in fresh cycles, and when stopping is usually discussed. We also note the monitoring debate and why policies differ by country.
Luteal Phase Support IVF — The 60‑Second Version
Why the luteal phase needs help after IVF
Stimulation and retrieval can blunt the corpus luteum. Progesterone supplements steady the lining while implantation is possible and early pregnancy starts.
The main routes at a glance
Vaginal micronised progesterone, IM progesterone in oil, subcutaneous aqueous progesterone, and oral dydrogesterone (availability varies). Some clinics combine routes.
Common mistake: switching routes mid‑cycle without clinic input
Always call your clinic before switching or adding a route. Many services can tailor within their protocol.
Evidence: ESHRE (2019 update; 2023–2024 practice notes) and Cochrane overviews report comparable outcomes across several routes in common protocols; individual trials vary.
Route‑by‑Route Comparison (Outcomes, Comfort, Access)
Vaginal progesterone (pessaries/gel)
Often first‑line. Local delivery to the endometrium with fewer systemic side‑effects. Common: discharge, irritation.
Intramuscular progesterone in oil (IM)
Long track record. Some patients and clinics prefer it. Cons: injection pain, nodules, site care.
Subcutaneous progesterone
Daily subcutaneous injections. Trials suggest similar effectiveness to IM in many settings with easier self‑administration. Local irritation possible.
Oral dydrogesterone
Used widely in some regions. RCTs and network meta‑analyses suggest non‑inferiority to vaginal in many protocols; availability and policy differ.
| Route | Effectiveness | Side‑effects | Convenience | Clinic preference | Notes |
|---|---|---|---|---|---|
| Vaginal | High (many RCTs) | Leakage, irritation | No needles | Common first‑line | Local delivery; combine in some clinics |
| IM (oil) | High (longstanding) | Injection pain, nodules | Needs assistance for some | Preferred in some centers | Durable track record |
| Subcutaneous | High (recent RCTs) | Local sting/itch | Self‑inject; no deep IM | Growing use | Similar outcomes to IM in many studies |
| Oral dydrogesterone | High (regional RCTs) | Systemic side‑effects rare | Very convenient | Region‑dependent | Policy and availability vary |
Evidence: 2024 network meta‑analyses and RCTs report similar clinical pregnancy/live birth across several routes; patient comfort and adherence differ (Cochrane 2021; updates 2024–2025).
Fresh vs FET — and Why Trigger Type Matters
Agonist trigger needs more intensive support
After a GnRH‑agonist trigger in fresh cycles, clinics often intensify luteal support or add low‑dose hCG carefully due to OHSS risk trade‑offs.
hCG trigger and OHSS considerations
hCG trigger supports the luteal phase but raises OHSS risk in high responders. Many clinics adjust support and consider freeze‑all in high‑risk cases.
Fresh transfer vs programmed/natural FET
Programmed FET relies fully on exogenous progesterone. Natural FET uses endogenous progesterone and may add supplementation. Timing is strict.
Evidence: ESHRE guidance (2019; practice notes 2023–2024) emphasises trigger‑specific support and OHSS‑aware planning; recent RCTs align on protocol‑driven choices.
When to Start and When to Stop
Typical start timing
Many clinics start on retrieval day or shortly after, and align the progesterone window with the planned transfer day.
When stopping is commonly considered
Many services continue until the first heartbeat scan or into early weeks of the first trimester; others stop earlier after a strong hCG rise. Protocols vary.
Mistake: self‑tapering without a plan
Do not reduce or stop without clinic direction. Call if side‑effects are tough so they can adjust safely.
Side‑Effects, Troubleshooting, and Adherence
Local irritation, leakage, injection pain
Pads for leakage, gentle site rotation, warm compresses for IM, and topical care for skin irritation. Ask your clinic before any changes.
Travel, refrigeration, logistics
Check storage rules. Build dosing into your daily routine. Carry a small kit for work or travel days.
When to call your clinic
Worsening symptoms, bleeding, rash or swelling, fever, or missed doses you cannot make up.
Comment: Which progesterone route did you choose—vaginal, IM, or subcutaneous—and what made it easiest for you?
Do You Need Progesterone Blood Tests?
Monitoring debate in plain English
Serum levels do not always mirror endometrial exposure. That is why clinics disagree about monitoring.
What some clinics do and why others don’t
Some check levels to catch very low outliers; others rely on protocol dosing and clinical milestones.
How to discuss monitoring
Ask what your clinic measures, thresholds they use, and what they will do with a result.
Evidence: Reviews note uncertain thresholds and weak correlation between single serum values and outcomes; policy is clinic‑specific (Cochrane; recent reviews 2023–2024).
Proof & Practicals
Mini case snapshot
Switched from IM to subcutaneous due to site pain. Outcomes were similar in the clinic’s data, and adherence improved.
Progesterone Route Comparison at a Glance
| Route | Pros | Cons | Who may prefer it |
|---|---|---|---|
| Vaginal | Local delivery, no needles | Leakage/irritation | Needle‑averse; travel light |
| IM | Long experience, clinician familiarity | Injection pain, nodules | Those comfortable with injections |
| Subcutaneous | Self‑administered, similar outcomes to IM | Local sting | Want predictable daily dosing without IM |
| Oral dydrogesterone | Convenient | Region/policy limits | Available markets with supporting protocols |
Talk to your clinic about luteal support (7 questions)
- Which route(s) do you recommend for me and why.
- How does my trigger type affect support.
- How will we time the start relative to retrieval/transfer.
- What side‑effects should I expect and how do I manage them.
- Will you monitor serum progesterone or not—and why.
- When might we stop if I have a positive test.
- What to do if I miss a dose or travel.
When to stop progesterone? (high‑level options)
Common options include stopping after a strong hCG trend, after the first heartbeat scan, or continuing to a set week in the first trimester. Follow your clinic plan.
FAQ
What is luteal phase support in IVF?
Which progesterone route works best?
Is subcutaneous progesterone as effective as IM?
Dydrogesterone vs vaginal—what does research say?
When should I start and stop progesterone after IVF?
Do I need progesterone blood tests?
Does trigger type change the plan?
Conclusion
Luteal phase support IVF comes in several routes with broadly similar effectiveness across many protocols. The best choice balances clinic protocol, trigger type, side‑effects, convenience, and access. Work with your team on start and stop timing, and ask about monitoring so the plan fits you.
Sources
- ESHRE: Ovarian stimulation for IVF/ICSI — includes trigger & luteal support (2019; updated notes) — core guideline; see ESHRE’s guideline hub for 2023–2024 practice updates and the 2025 stakeholder update draft.
- Cochrane: Luteal phase support for assisted reproduction (overview) — comparative evidence across progesterone routes and regimens; see Cochrane Gynaecology & Fertility for related updates.
- Three-arm RCT: vaginal vs subcutaneous vs intramuscular in FET (2024).
- Network meta-analysis of LPS routes after fresh ET (2025).
- Prospective RCT: oral dydrogesterone + vaginal vs vaginal alone (2024) — combo not superior to vaginal alone.
Reminder: Follow your clinic’s luteal support protocol. Do not change dose or route without clinician guidance.