Featured answer
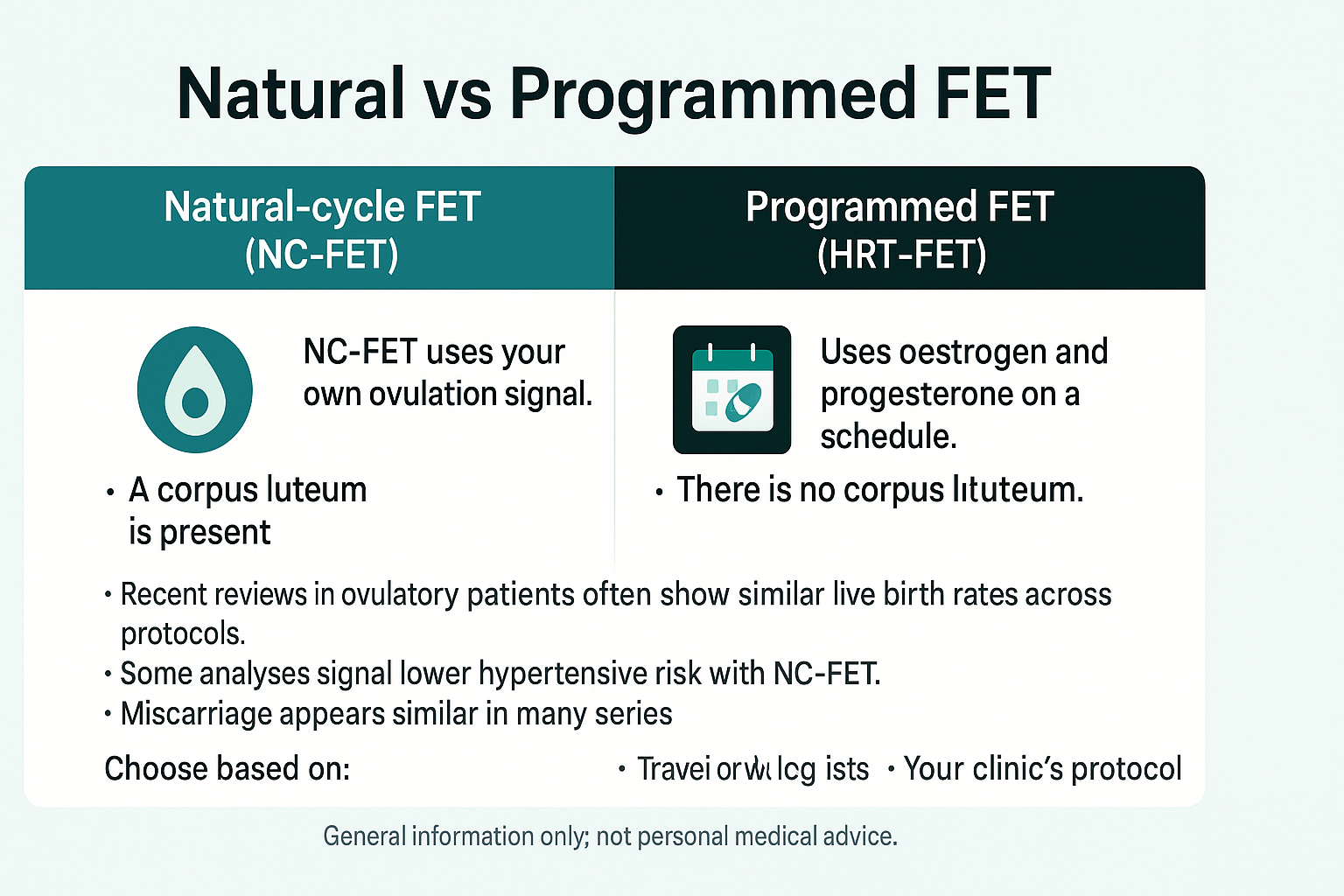
Natural vs programmed FET in plain English. NC‑FET uses your own ovulation signal. A corpus luteum is present. HRT‑FET uses oestrogen and progesterone on a schedule. There is no corpus luteum. Recent reviews in ovulatory patients often show similar live birth rates across protocols. Some analyses signal lower hypertensive risk with NC‑FET. Miscarriage appears similar in many series. The best choice depends on ovulation reliability, monitoring tolerance, travel or work logistics, and your clinic’s protocol.
Introduction
You want the safest plan that also fits your life. Natural vs programmed FET is a real trade‑off between biology and convenience. This guide gives a clear, evidence‑based map without jargon.
We explain the corpus luteum, outcomes that matter, who fits each protocol, the logistics of monitoring and meds, and red flags that need fast care. You can also print a planner for HRT schedules.
Natural vs Programmed FET in 60 Seconds
NC‑FET: spontaneous LH or modified with hCG, corpus luteum present
True NC tracks your LH surge. Modified NC adds an hCG trigger to time progesterone and transfer. A corpus luteum is present to make hormones and vasoactive factors.
HRT‑FET: oestrogen plus progesterone on a fixed schedule, no corpus luteum
Your team builds the lining with oestrogen and then adds progesterone to match the embryo’s age. It can be easier to schedule and to line up lab capacity.
Common mistake: assuming medicated always means better outcomes
Control helps planning, but outcomes depend on more than scheduling. Reviews do not show a universal live‑birth advantage for HRT‑FET in ovulatory patients.
Evidence: Human Reproduction Update 2023 and Cochrane 2025 update summarise similar live birth across protocols in ovulatory cohorts, with protocol choice guided by eligibility and service setup.
Outcomes That Matter
Live birth
Most pooled analyses in ovulatory patients find similar live birth for NC‑FET and HRT‑FET. Individual clinic data can differ.
Miscarriage and early loss
Rates are broadly comparable in many reviews. Differences are small and often not consistent between studies.
Hypertensive disorders in pregnancy
Signals from observational cohorts and some trials suggest lower hypertensive risk with NC‑FET, possibly due to corpus luteum factors that support vascular adaptation.
Evidence: A recent PLOS Medicine trial and large cohorts report lower hypertensive disorder rates with corpus luteum presence. Mechanism theories include vasoactive peptides from the corpus luteum.
Who Is a Candidate for Each Protocol?
NC‑FET likely candidates
Regular ovulation, comfort with tracking or frequent checks, and flexibility to attend monitoring.
HRT‑FET likely candidates
Anovulation or very irregular cycles, donor eggs, need for precise scheduling, or travel constraints. Some clinics prefer HRT for lab scheduling.
Edge cases to discuss
PCOS with irregular ovulation, short luteal phases, or time‑zone and shift‑work challenges.
Evidence: Human Reproduction Update reviews outline candidate selection by ovulation status and service organisation.
Logistics and Lifestyle: Monitoring vs Convenience
Appointments and tests
NC often needs more scans and bloods to catch the LH rise and confirm timing. HRT uses fewer visits with a planned start.
Medication load, side‑effects, and adherence
NC may use little or no oestrogen. HRT uses oestrogen and progesterone on a schedule. Choice of route for progesterone affects comfort.
Work, travel, and time‑zones
HRT can be easier to time around travel or work rosters. NC can work well if you can attend flexible monitoring.
Did your clinic prefer natural or programmed, and what tipped the decision for you?
Medication Plans and Luteal Support
NC‑FET luteal support
Some clinics add progesterone after ovulation. Others do not if luteal function looks strong. Policies differ.
HRT‑FET timing and dosing principles
Your team sets oestrogen buildup and then starts progesterone to match the embryo age. Do not change dose or route without clinical advice.
Common mistake
Switching route or dose on your own. Always call first so the plan stays aligned with timing.
Evidence: ESHRE practice resources describe multiple acceptable luteal approaches and stress clinic protocol consistency.
Safety: Red Flags and When to Call
Urgent symptoms
Heavy bleeding, severe or one‑sided pain, faintness, shortness of breath, severe headache, or visual changes.
What clinics may do next
Blood tests, blood pressure checks, and ultrasound to confirm location and wellbeing.
Do not wait with severe symptoms
Seek care quickly. Tell staff your transfer date and medicines.
Putting It Together: A Simple Decision Map
If you ovulate reliably and can attend monitoring
NC‑FET is often feasible and may carry lower hypertensive risk in some analyses.
If cycles are irregular or timing is critical
HRT‑FET is often practical and easier to schedule with your clinic and lab.
Shared decision checklist
- Do I ovulate regularly.
- Can I attend monitoring at short notice.
- What are my travel or work constraints.
- What does my clinic’s data show.
- How do they manage luteal support in each protocol.
- What risks and side‑effects matter most to me.
- What is the backup plan if timing slips.
Proof and Practicals
Mini case snapshot
Regular ovulator chose NC and liked fewer meds. A shift worker chose HRT to control timing. Both reached similar outcomes in their clinic data.
NC‑FET vs HRT‑FET at a Glance
| Aspect | NC‑FET | HRT‑FET |
|---|---|---|
| Live birth (ovulatory) | Similar in many reviews | Similar in many reviews |
| Miscarriage | Often similar | Often similar |
| Hypertensive disorders | Lower signal in some studies | Higher signal in some studies |
| Monitoring | More scans/bloods | Fewer visits |
| Meds | Minimal or progesterone only | Oestrogen plus progesterone |
| Convenience | Flexible but requires attendance | Scheduling is simpler |
Questions to ask about your FET plan
- Which protocol fits my ovulation pattern.
- How many visits will I need.
- What progesterone route will we use.
- Are there hypertension signals I should know about.
- What are the red flags and who do I call.
- Can I use the Medication & Injection Planner (print‑only).
- Where can I read more: FET protocols explained.
FAQ
Is natural‑cycle FET better than programmed FET?
Does NC‑FET lower hypertension risk in pregnancy?
Which protocol has higher live birth rates?
Who should not do a natural‑cycle FET?
Do I need luteal support with NC‑FET?
How many appointments do I need for each protocol?
Can I switch from HRT to NC next cycle?
Conclusion
Natural vs programmed FET is about fit and safety. In ovulatory patients, live birth is often similar across protocols, with a possible lower hypertensive risk signal for NC‑FET. Your best choice balances ovulation reliability, logistics, and your clinic’s protocol.
Sources
- Cochrane Review: Cycle regimens for endometrial preparation prior to FET (2025 update) — global evidence comparing natural vs programmed protocols and logistics.
- Human Reproduction Update: Secretory products of the corpus luteum and preeclampsia (review) — physiology of the corpus luteum and links to hypertensive outcomes in programmed FET.
- PLOS Medicine RCT: Natural vs HRT endometrial prep in ovulatory women (COMPETE, 2025) — randomized trial reporting live birth and obstetric outcomes; printable PDF available.
- ESHRE practice resources: Embryo transfer guideline (clinic pathways & luteal notes) — practical recommendations relevant to protocol selection and support.
Reminder: Choose your FET protocol with your fertility team. Seek urgent care for severe pain, heavy bleeding, faintness, or severe headache or visual changes.