Quick answer
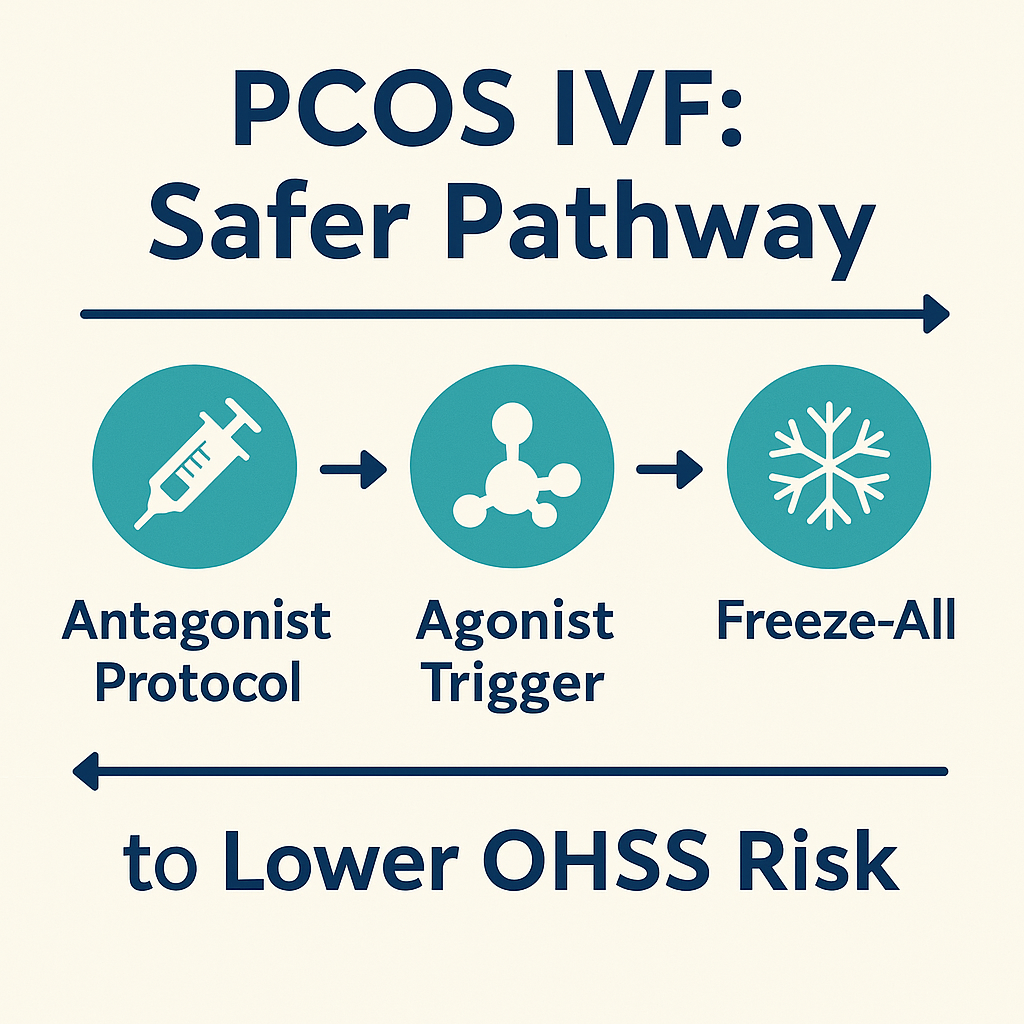
For most people with PCOS, a safer PCOS IVF plan is a GnRH antagonist protocol with a GnRH agonist trigger, personalised FSH dosing, and a freeze‑all strategy when OHSS risk is high. Add cabergoline and supportive steps where appropriate. Monitor daily after trigger and call your clinic if red flags appear.
Introduction
Many people fear OHSS and feel lost in protocol names. PCOS IVF does not need to be a maze. This guide shows why the antagonist protocol plus an agonist trigger and freeze‑all can lower risk, when to use it, and how to choose FET timing. We keep the language simple and the steps clear.
PCOS IVF at a Glance
Why PCOS changes the plan
PCOS often comes with high AMH and a large antral follicle count. Ovaries can be sensitive to FSH. The goal is enough eggs without tipping into OHSS.
The safer trio
Antagonist protocol. Agonist trigger. Freeze‑all when risk is high. This trio cuts the biggest OHSS drivers while keeping good outcomes.
Common mistake
Chasing high egg counts. More eggs can mean more risk and no extra benefit.
Evidence: ESHRE PCOS guidance (2023) and ASRM OHSS prevention statements (2023–2024) support antagonist cycles, agonist triggers, and cycle segmentation to reduce OHSS.
Risk Stratification Before You Start
Key risk factors
Very high AMH or AFC, prior OHSS, very rapid oestrogen rise, and a strong response on low FSH. BMI is not a moral metric. It is one of many clinical factors.
Baseline labs and ultrasound
Agree a starting FSH dose that is conservative. Adjust based on scans and bloods. Use one lab when possible.
Mistake to avoid
One‑size‑fits‑all FSH starts. Personalise from day one.
Evidence: Reviews show individualised FSH dosing reduces overstimulation in PCOS and high responders (recent RCT summaries).
Stimulation Protocols for PCOS
Antagonist protocol
Short, flexible, and blocks LH surges. It allows the safer agonist trigger. That is why it is common in PCOS IVF.
Mild stimulation and coasting
Lower daily doses can reduce risk. Coasting is a short pause when levels climb too fast. Your team decides if and when to use it.
Add‑ons with some evidence
Metformin in selected people. Cabergoline around trigger in high‑risk cases. Ask your team what fits your history.
Evidence: ASRM and ESHRE list metformin and cabergoline among options for high‑risk responders; evidence varies by study.
Trigger Choices and Immediate Aftercare
Agonist trigger vs hCG trigger
Agonist trigger causes a short LH surge and lowers late OHSS risk. hCG trigger lasts longer and can fuel OHSS in high responders.
Luteal support after agonist trigger
Support often needs to be stronger or adjusted. Your clinic will outline the plan.
Watch for late OHSS
Risk can rise after retrieval. Keep daily notes for a week and call early if symptoms grow.
Preventing OHSS Step by Step
During stimulation
Start low. Titrate based on scans and oestradiol. Consider coasting when thresholds are met.
At trigger
Prefer an agonist trigger. Consider cabergoline. Your team may discuss fluids or albumin in selected cases.
After retrieval
Weigh daily. Track waist size, urine, and symptoms. Know the red flags and when to call.
Comment: What protocol did your clinic recommend—antagonist with agonist trigger or something else, and why?
Why Freeze‑All Can Be Wise in PCOS
How it cuts OHSS
Pregnancy hormones can worsen OHSS. Freezing embryos and delaying transfer reduces that risk.
When to freeze‑all
If response is very strong or symptoms start, freezing can be safer. Your team will tell you if this is the plan.
Fresh transfer under high risk
Avoid forcing a fresh transfer when risk is high. Safety first.
FET Choices for PCOS (Timing & Prep)
Natural‑cycle vs HRT‑prepped FET
Natural cycles use your own ovulation. HRT cycles use oestrogen and progesterone. Your history and clinic workflow guide the choice.
Monitoring and timing
For natural cycles, ovulation timing matters. For HRT cycles, progesterone start sets transfer day.
Delay if needed
If risk was high or recovery slow, wait a cycle. Healing helps.
Red Flags—Call the Clinic Now
Urgent symptoms
Rapid weight gain, new or marked abdominal swelling, severe pain, shortness of breath, low urine, dizziness or faintness.
What the clinic may do
Bloods and ultrasound. Advice on fluids. Sometimes day‑stay care or admission.
Do not wait
If symptoms grow fast, call now.
Proof & Practicals
Mini case snapshot
High‑AMH person used an antagonist protocol with an agonist trigger and froze all embryos. Recovery was steady. HRT‑prepped FET the next cycle led to a healthy ongoing pregnancy.
PCOS IVF Safety Toolkit
| Step | Action | Why it helps |
|---|---|---|
| Protocol | GnRH antagonist | Enables safer agonist trigger |
| Trigger | GnRH agonist | Cuts late OHSS risk |
| Add‑on | Cabergoline (selected cases) | Blunts VEGF‑mediated leak |
| Dose | Individualised FSH | Avoids overstimulation |
| Segmentation | Freeze‑all when high risk | Avoids pregnancy‑worsened OHSS |
| Aftercare | Daily checks for a week | Finds early red flags |
Your OHSS Prevention Plan
- Agree a conservative start dose and monitoring dates.
- Learn your clinic’s coasting and trigger thresholds.
- Use an agonist trigger if risk is high.
- Ask about cabergoline and luteal support.
- Prepare for freeze‑all if advised.
- Track weight, waist, urine, and symptoms after retrieval.
- Call early if red flags appear.
Useful links
- Injection planner (print-only) — simple printable schedule to map daily stimulation and trigger injections.
Sources
- ESHRE: PCOS guideline (2023) — European Society of Human Reproduction and Embryology clinical guideline.
- ASRM: OHSS prevention guidance (2023–2024) — American Society for Reproductive Medicine recommendations.
- Peer-reviewed RCT and review summaries on antagonist cycles, agonist triggers, and cabergoline in high responders (various years) — academic evidence base.
FAQ
What is the safest IVF protocol for PCOS?
Does a GnRH agonist trigger prevent OHSS?
When should I freeze‑all?
Is metformin helpful for PCOS IVF?
Which FET approach works best in PCOS?
What symptoms mean OHSS could be starting?
How long should I wait for FET after high risk?
Conclusion
PCOS IVF is safest when you focus on risk first. Antagonist protocol, agonist trigger, and freeze‑all where needed form a strong base. Then choose FET timing that fits your body and clinic. Share what worked for you so others can plan.
Reminder: If you have severe pain, fast weight gain, or shortness of breath after trigger or retrieval, contact your clinic or emergency care.