Featured answer
PGT‑A is a screening test, not a diagnosis. It samples outer cells (trophectoderm) from a blastocyst and uses next‑generation sequencing to look for chromosomal copy‑number changes. Pros: may reduce transfers of aneuploid embryos and shorten time to pregnancy in selected groups. Cons: not 100% accurate; mosaic and segmental results add complexity; cost varies. Mosaic results need counseling and do not force embryo disposal.
Introduction
Choosing add‑ons is stressful. You want clear facts. This guide lays out PGT‑A pros and cons in plain English. We cover ASRM 2024 points, mosaic embryo transfer basics, and PGT‑A accuracy limits. Use it to frame questions for your team and your genetic counselor.
PGT‑A in One Page
What it is
Screening for chromosomal copy‑number changes in embryos. It is not diagnostic. If pregnant, prenatal testing is still recommended.
How it is done
Trophectoderm biopsy on a day‑5/6 blastocyst, followed by NGS. The result is a snapshot of sampled cells, not the whole embryo.
Common mistake
Assuming a “normal” report means zero risk or that a “mosaic” report means discard. Both views are too simple.
Evidence: ASRM committee opinion 2024 and ESHRE guidance summaries note screening intent and the need for prenatal confirmation.
PGT‑A Pros and Cons (At a Glance)
Potential benefits
Selected groups may see fewer aneuploid transfers and a shorter time to pregnancy. PGT‑A can reduce transfers that would likely fail due to whole‑chromosome aneuploidy.
Key limitations
No universal live birth gain across all ages. False calls can occur. Segmental changes and mosaicism raise uncertainty. Cost and access vary by region.
Who may benefit vs who may not
People with many embryos to choose from or with advanced maternal age may see value. With very few embryos, the cost–benefit often shifts. Prior losses and history matter.
| Point | What it may help | What it can’t promise |
|---|---|---|
| Reduce aneuploid transfers | Fewer non‑viable transfers | Does not remove all risk |
| Time‑to‑pregnancy | May shorten in select groups | Not universal across ages |
| Miscarriage risk | May reduce in some groups | Pregnancy still needs confirmation |
| Cost‑effectiveness | Better when embryo numbers are higher | Often poorer with few embryos |
Evidence: Non‑selection studies and reviews show mixed live birth effects across ages; benefits are clearer for time to pregnancy in selected groups.
Accuracy, Errors, and What Labs Actually Report
Copy‑number calls and thresholds
Reports classify whole‑chromosome or segmental gains/losses. Labs use thresholds to call euploid, mosaic, or aneuploid. Thresholds vary by lab.
False positives/negatives; TE vs ICM
Sampling error and technical noise can create false calls. TE biopsy may not match the inner cell mass. This is why counseling is essential.
Why non‑selection studies matter
They reduce selection bias and show that PGT‑A does not guarantee higher live birth rates for everyone. It helps frame realistic expectations.
Evidence: ASRM 2024 and recent reviews discuss discordance between TE and ICM and the need for cautious interpretation.
Mosaic Embryos, Explained
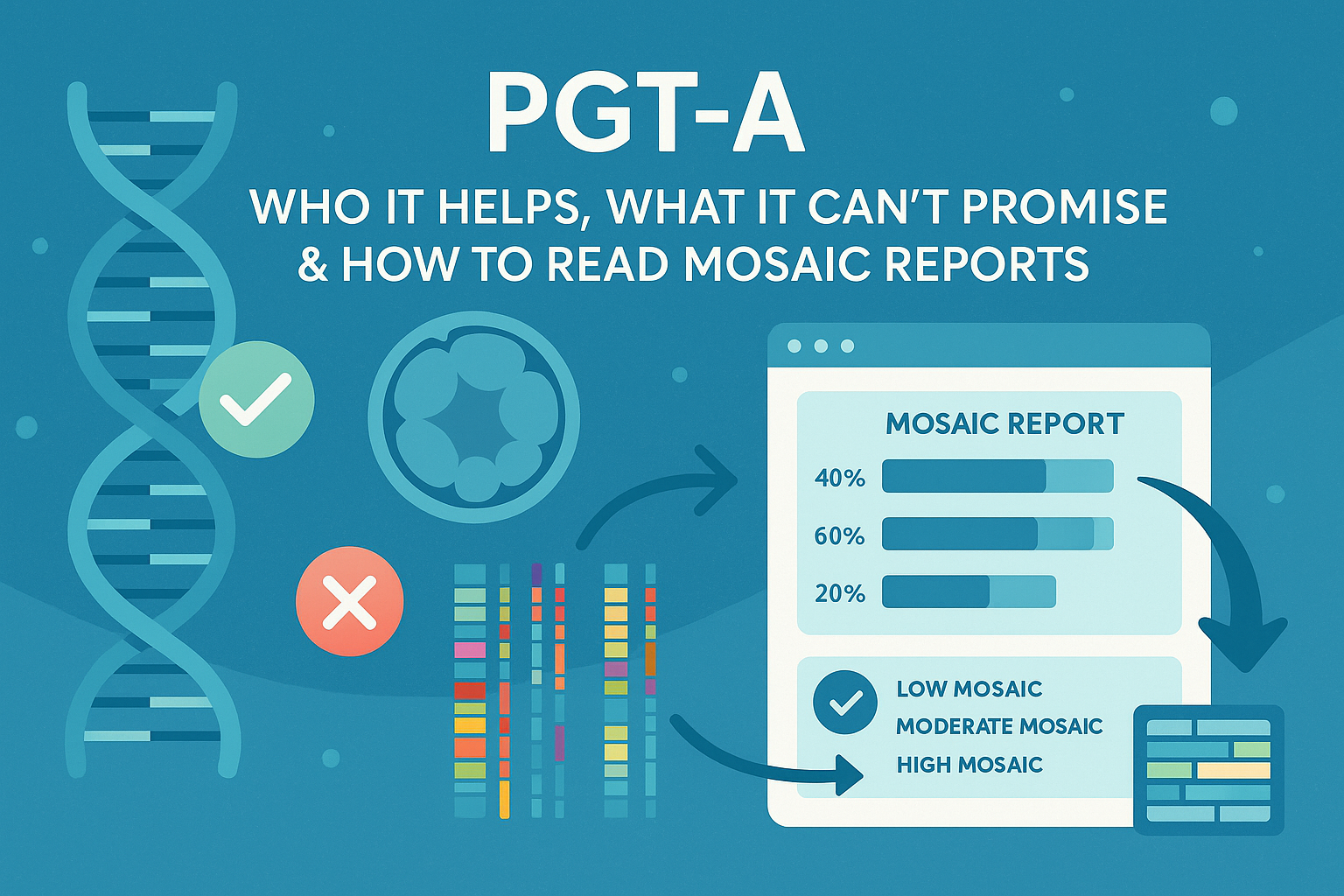
What “mosaic” means
Two or more cell lines with different chromosome content. Labs often report low‑ vs high‑level mosaic categories based on percentage bands.
How to read a mosaic report (steps)
- Note the chromosome(s) and whether it is whole or segmental.
- Note the mosaic band (for example, 20–40% vs 40–80%—lab dependent).
- Ask for the lab’s transfer policy and prioritisation.
- Book genetic counseling to discuss uncertainty and prenatal testing plans.
- Do not make embryo disposition decisions without full counseling.
Outcomes and uncertainty
Many clinics consider low‑level mosaics for transfer after counseling. Outcomes vary and depend on the specific finding and the person’s history.
Evidence: ESHRE and peer‑reviewed studies report transfers of selected mosaics with cautious outcomes; policies differ by clinic.
What ASRM (2024) and ESHRE Highlight
Consensus points
Screening, not diagnosis. Benefits in selected settings. Prenatal confirmation if pregnant. Counseling for mosaic or complex reports.
Where guidance is cautious
Live birth advantage is not universal. Segmental and high‑level mosaic results require careful interpretation.
Prenatal confirmation
If pregnancy occurs, CVS or amniocentesis is recommended to confirm. NIPT is screening and may not resolve all concerns.
Costs, Trade‑Offs, and Ethics
Cost vs expected value
Value improves when embryo numbers are higher. It often declines when embryos are few. Regional pricing and access differ.
Non‑directive framing
Your values and risk tolerance matter. This is a decision with trade‑offs. The best choice is shared with your team.
Equity and access
Consider access and cost barriers. Ask about financial consent and written quotes.
Decision Checklist (Print‑Friendly)
Seven questions to ask
- What is my per‑embryo chance with and without PGT‑A.
- How many embryos do I likely have.
- What is the plan if reports come back mosaic or no‑call.
- What are the lab’s thresholds and categories.
- What is the policy for transferring low‑level mosaics.
- What prenatal testing will be offered if pregnant.
- What is the total cost and timeline.
How embryo number changes the math
More embryos usually improve sorting value. With very few embryos, sorting value may be low and cost can dominate.
Plan for outcomes
Write down actions for euploid, mosaic, and no‑call before testing starts. It reduces panic later.
Comment: What did your clinic say about PGT‑A—helpful, optional, or not needed for you?
Proof & Practicals
Mini case snapshot
One person with many embryos used PGT‑A and transferred a euploid on the first attempt. Time to pregnancy was short. Another with two embryos used PGT‑A, received one mosaic and one no‑call, and chose counseling before deciding. Different value, different plan.
Flow: how to read a mosaic report
- Identify chromosome and type (whole vs segmental).
- Check the mosaic band.
- Review clinic policy on mosaic transfers.
- Meet a genetic counselor.
- Decide on next steps with your team.
Checklist — before authorising PGT‑A
Confirm consent language, reporting categories, handling of mosaic/no‑call, costs for rebiopsy if offered, and prenatal testing plan if pregnant.
Useful links
- PGT‑A for beginners: https://ivftoolkit.com/blog/pgt-a-beginners
- Mosaic embryo: https://ivftoolkit.com/glossary/mosaic
Sources
- ASRM Committee Opinion on PGT‑A, 2024. https://www.asrm.org
- ESHRE guidance and working group notes on PGT‑A, 2023–2024. https://www.eshre.eu
- Recent non‑selection and concordance studies on TE vs ICM and outcomes (various years).
FAQ
Is PGT‑A diagnostic or screening?
Who benefits most from PGT‑A?
How accurate is PGT‑A and what can it miss?
What does mosaic mean and how should I decide?
Does PGT‑A lower miscarriage for everyone?
Can a ‘no‑call’ embryo be rebiopsied?
What do ASRM (2024) and ESHRE recommend today?
Do I still need CVS/amnio after PGT‑A?
Conclusion
PGT‑A pros and cons are easiest to weigh when you see the limits of screening, the value of time saved in some groups, and the uncertainty around mosaic results. Use counseling and plan for prenatal confirmation if pregnant. Choose with your team.
Reminder: Discuss PGT‑A and any mosaic results with your fertility specialist and a genetic counselor before making decisions.