Featured answer
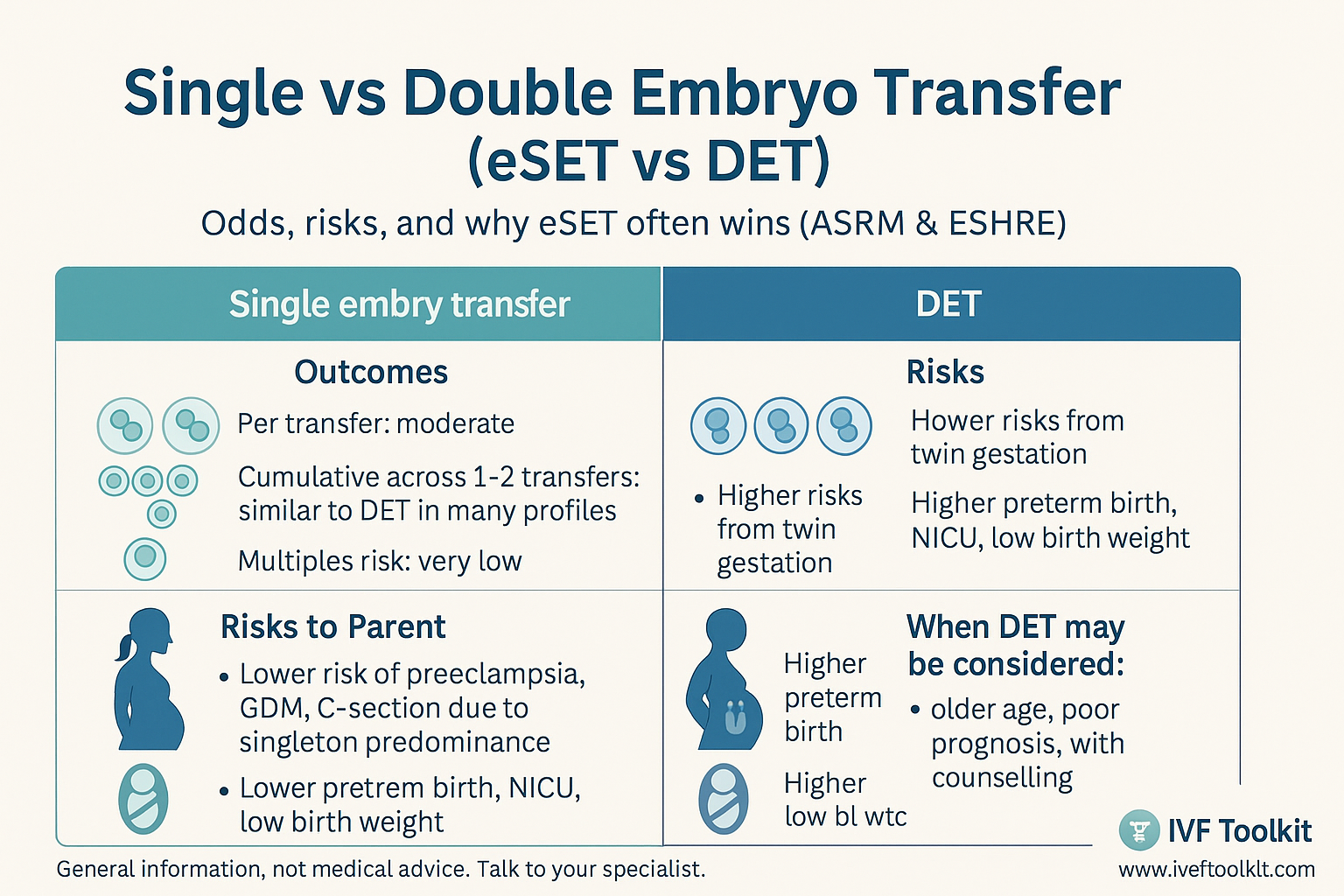
Single embryo transfer means placing one embryo. Double embryo transfer means placing two. The trade off is simple. eSET lowers the chance of twins and the risks that follow while keeping similar cumulative outcomes across one to two transfers in many groups. DET may lift per transfer odds but raises multiple pregnancy risk. Most clinics start with eSET for safety.
Introduction
You want the best chance and the safest plan. Single embryo transfer is the choice many clinics lead with. eSET vs DET is about risk and timing. We set out the odds per transfer and across a short series and explain why the lower twin risk often wins. You will also see what ASRM and ESHRE suggest today.
Single vs Double Embryo Transfer at a Glance
Definitions and quick context
Single embryo transfer is one embryo in the uterus. Double embryo transfer is two. Results depend on age, embryo stage and quality, and clinic practice.
The three numbers that matter
Per transfer success. Cumulative success across one to two transfers. Risk of multiple pregnancy. Cumulative is the number many people care about and it is often similar with eSET when a second transfer is used if needed.
Common mistake
Chasing twins to save time. Twin pregnancies carry higher risks to mother and babies. That is why many clinics set eSET as default.
Evidence: ASRM guidance (2023) and ESHRE guidance (2023–2024) support eSET for good prognosis groups to cut multiple pregnancy without lowering cumulative live birth.
Odds and Outcomes
Per transfer vs cumulative
DET can raise per transfer pregnancy rates. eSET across one to two transfers can reach similar cumulative live birth in many groups while holding a much lower twin rate. This is the key safety win.
Age, embryo stage, and quality
Younger age and high quality day 5 embryos favour eSET. Older age or lower quality may change the numbers and the discussion. Cleavage stage embryos have different performance to blastocysts.
PGT‑A and how it shifts decisions
If a euploid embryo is available, many clinics prefer eSET because the per embryo odds are higher and the twin risk is lower with one.
Evidence: Peer reviewed studies show higher risks with multiples, including preterm birth and low birth weight. Cumulative outcomes can be similar with eSET plans that allow a second transfer.
Risks of Multiple Pregnancy
Maternal risks overview
Higher rates of preeclampsia, gestational diabetes, anaemia, operative birth, and postpartum haemorrhage are seen with twins.
Baby risks overview
Higher rates of prematurity, low birth weight, NICU time, and longer stays are seen with twins. Long term outcomes are linked to gestation and weight.
Health system and cost impacts
Multiple pregnancies increase use of antenatal visits, scans, admissions, and neonatal care. This matters for families and health systems.
Evidence: ASRM and ESHRE note consistent risk increases with multiple gestation. Reducing twins is a shared goal.
What ASRM and ESHRE Say
High level guidance by age and embryo quality
Good prognosis groups are encouraged to choose eSET. For older age brackets or when embryo quality is low, the number transferred may change after counselling. Policies vary across regions.
When DET may be considered
Some clinics consider DET after discussion when prognosis is poor and embryo quality is low. The decision is documented and risks are explained.
Why many clinics default to eSET
It protects safety while keeping similar cumulative outcomes for many groups across short series of transfers.
Evidence: ESHRE overview 2023 and ASRM committee opinions 2023 report lower multiple rates with eSET with similar cumulative live birth across planned repeats.
Fresh vs Frozen, Day 3 vs Day 5
Practical differences that affect choice
Day 5 transfers often have higher per embryo performance. Frozen cycles allow time for screening and recovery. Local practice and lab skill matter.
Lab and clinic variation notes
Success varies by programme. Your team’s data help set the baseline for you.
Common myths to skip
Two embryos do not simply double your chance. They do increase the chance of twins and the risks that follow.
Shared Decision Checklist
Questions to ask your clinic
What are my per transfer and cumulative odds with one vs two. What twin rate applies here. What is the plan if the first eSET does not work.
Values and risk tolerance prompts
How do I weigh a small gain in speed against a larger rise in twin risk. How do I feel about possible prematurity or NICU care.
Red flags and when to pause
If your health risks are high, ask if eSET is strongly preferred. If the clinic cannot show current data, ask for it.
Proof and practicals
Mini case snapshot
A person chose eSET with a high quality blastocyst. The first transfer failed. The second worked. One healthy baby. Another person chose DET with similar embryos and became pregnant with twins. Birth was preterm and the stay in hospital was longer. Different stress profiles. Discuss what fits you.
eSET vs DET at a glance
| Factor | eSET (single) | DET (double) |
|---|---|---|
| Per transfer odds | Lower than DET in many groups | Higher per transfer |
| Cumulative across 1–2 transfers | Often similar to DET | Often similar to eSET |
| Multiple pregnancy risk | Low | Higher |
| Recovery burden | Lower | Higher if twins |
| Costs over time | Can be similar if second transfer used | Can be higher with twin care |
| Guideline stance | Often preferred for safety | Considered only in selected cases |
Checklist before you choose 1 or 2 embryos
- Ask for per transfer and cumulative odds in your age band.
- Ask for twin rates with one vs two.
- Confirm embryo stage and quality and if PGT‑A was done.
- Ask the plan if the first eSET fails.
- Consider health risks if pregnant with twins.
- Check clinic policy and local rules.
- Write down your values and limits.
Myth vs Fact
Myth: Two embryos always double your chance.
Fact: Two can lift per transfer odds. They also lift twin risk. Cumulative outcomes can be similar with eSET and a plan for a second transfer.
Useful links
- Follicle & Lining Visualizer — chart follicle growth and endometrial thickness, track OLS trends, and generate a printable report.
- Cycle Day & Fertile Window — maps LMP to fertile window and ovulation; for IVF: stims → trigger → transfer.
- IVF twins risks — article on risks and considerations with multiple embryo transfer.
Sources
- ASRM: Committee guidance on number of embryos transferred (2023) — American Society for Reproductive Medicine recommendations.
- ESHRE: Embryo transfer guideline overview (2023–2024) — European Society of Human Reproduction and Embryology guidance.
- Peer-reviewed reviews on multiple pregnancy risks and neonatal outcomes (various years) — academic literature synthesis.
FAQ
Is single embryo transfer safer than double?
Do two embryos always raise success rates?
When might DET be reasonable?
How do age and embryo quality change the plan?
Does PGT‑A make eSET the default?
What are the main risks of twins in IVF?
What do ASRM and ESHRE recommend today?
Conclusion
Single embryo transfer often gives the safest path with similar cumulative success across short series of transfers. It lowers the risk of twins and the problems that follow. Discuss your numbers, embryo quality, and values with your team and use the checklist to decide well.
- What did your clinic recommend and why. Share your situation to help others.
- Read our guides on embryo transfer choices and twin risks next.
Reminder: Discuss embryo number with your fertility specialist. Your age, embryo quality, and health history matter.